Microbial Management
From the Series: Embodied Ecologies
From the Series: Embodied Ecologies
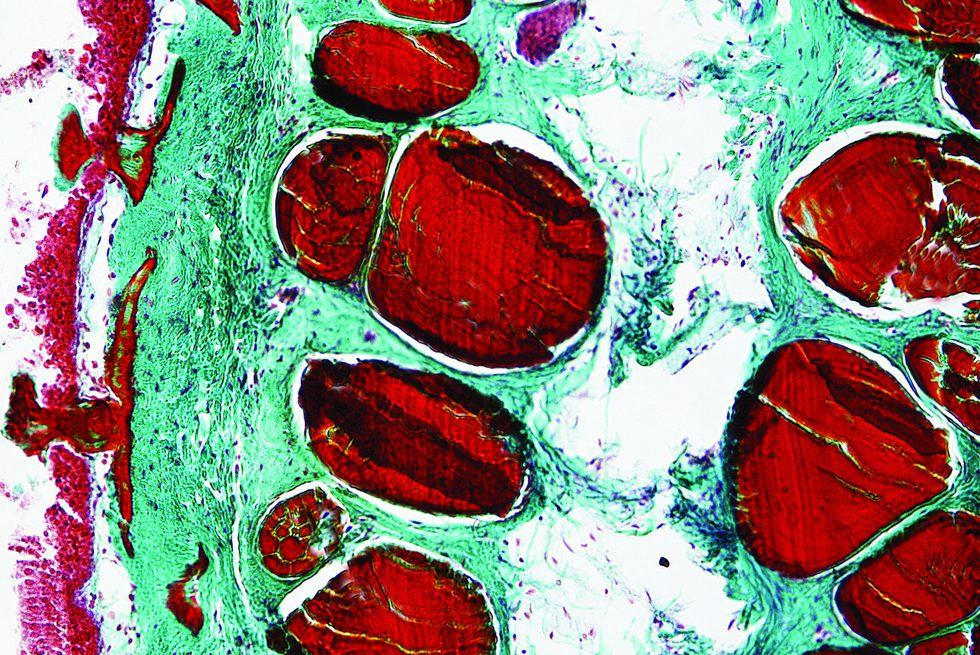
“I think gut flora [chōnai furo-ra] is really important to health and to food allergies,” said Tomoko, a woman in her late forties and the mother of a multiply allergic child. “Our doctor’s methods are about that. He says to eat lots of fiber, organic food, no additives or preservatives, not much meat, and lots of fermented and pickled foods—a traditional Japanese diet. We are trying to reset the gut and then see what happens,” she continued. Tomoko referred here to the microbiome, a focus of medical and social scientific research in recent years. Microbes are essential for human health, and they are increasingly understood as part and parcel of what a human is. Dorion Sagan (2013, 17), for example, argues that “humans are more than human,” while other scholars invoke figures of superorganisms and holobionts (Lorimer 2016, 2018). Stefan Helmreich (2015), meanwhile, diagnoses a turn to the microbial human: homo microbis instead of homo sapiens.
Participants in Japanese food allergy patient support communities discuss and debate ideas about gut health, often couched in terms like gut flora (chōnai furo-ra) and gut bacteria (chōnai saikin), with positions heavily influenced by their physicians. As one woman expressed to me: “It’s like beliefs, almost like a religion. It depends on the doctor.” Those who adhere to a method of microbial management focus on understanding and nurturing their internal microbial communities. They hope that changing food and bodily environments will eliminate, mitigate, or reduce allergic reactions at some point in the future. Adherents look to medical research that explores the potentially positive effects of probiotics on oral immunotherapy outcomes (e.g., Tang et al. 2015) and other linkages between allergies and the microbiome.
To espouse the view that adapting gut health can mitigate allergic reactions is to commit to a daily regime of time- and labor-intensive practices. The doctor of the woman quoted in the previous paragraph is well-known—and controversial—in allergy circles in Japan for his emphasis on eating a traditional Japanese diet of fermented, pickled, organic food instead of prepackaged ready meals: an approach that we might call microbiocultural. It relies not only on the notions of a national diet rich in microbial offerings and of environmentally entangled and adaptive bodies, but also on the domestic labor of (usually) women to make it possible—as well as the financial resources to buy organic produce and to be at home to make meals. Tomoko, whose daughter has multiple allergies, expressed her commitment to this ideal but also confessed her exhaustion at having to prepare everything from scratch for three meals a day. It was sometimes so tiring that she had been thinking about changing their doctor and approach. Her husband, adamant that they had decided to trust their physician, was determined that they should continue.
As I have discussed elsewhere, maintaining gut health is common sense for much of the food allergy patient support community in Japan. Gut microbes are understood within a wider body of received knowledge relating to gut health, which is informed by a range of media from health-related television programs to advertisements for fermented supplements like Shin-Bioferumin: a powder consisting of three different types of bacteria. There are consequently ongoing “local biologies” (Lock 2017, 5) that explicitly bring together various imaginaries and understandings of microbes, bodies, and health.
However, many food allergy parents await clinical evidence demonstrating the efficacy of microbial management practices before taking them up. Indeed, many doctors caution that there are so many microbial strains that it is, as of yet, difficult to know which ones may be beneficial and in what quantities. Moreover, what works well for one person may not work for another.
Yet some parents in Japan, like Tomoko, are using microbes as a technology of management, acting on the hypothesis—and hope—that reconfiguring the microbiome will reconfigure bodies such that children may grow out of their allergies. In this approach, the quality, variety, and condition of both individual and familial microbial communities is being attended to and encouraged to develop. Here, microbiopolitics, microbiosociality (see Paxson 2008), and microbiocuturalism are all in play.
Helmreich, Stefan. 2015. Sounding the Limits of Life: Essays in the Anthropology of Biology and Beyond. Princeton, N.J.: Princeton University Press.
Lock, Margaret. 2017. “Recovering the Body.” Annual Review of Anthropology 46: 1–14.
Lorimer, Jamie. 2016. “Gut Buddies: Multispecies Studies and the Microbiome.” Environmental Humanities 8, no. 1: 57–76.
_____. 2018. “Hookworms Make Us Human: The Microbiome, Eco-Immunology, and a Probiotic Turn in Western Health Care.” Medical Anthropology Quarterly 33, no. 1: 60–79.
Paxson, Heather. 2008. “Post-Pasteurian Cultures: The Microbiopolitics of Raw-Milk Cheese in the United States.” Cultural Anthropology 23, no. 1: 15-47.
Sagan, Dorion. 2013. Cosmic Apprentice: Dispatches from the Edge of Science. Minneapolis: University of Minnesota Press.
Tang, Mimi L. K., Anne-Louise Ponsonby, Francesca Orsini, Dean Tey, Marnie Robinson, Ee Lyn Su, Paul Licciardi, Wesley Burks, and Susan Donath. 2015. “Administration of a Probiotic with Peanut Oral Immunotherapy: A Randomized Trial.” Journal of Allergy and Clinical Immunology 135, no. 3: 737–44.