Hospital Diaries: Experiences with Public Health in Sierra Leone
From the Series: Ebola in Perspective
From the Series: Ebola in Perspective
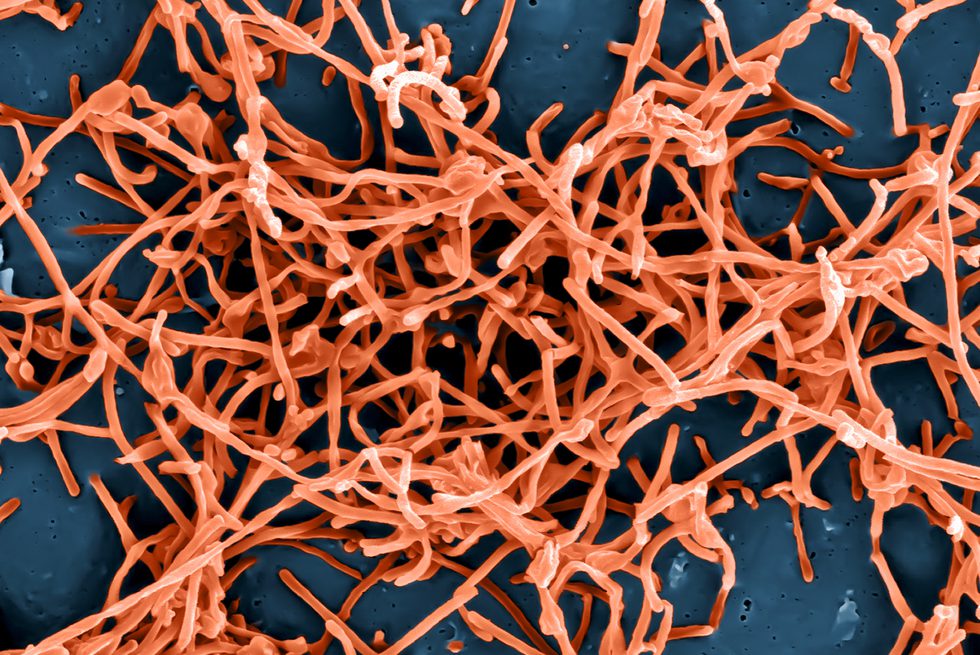
Early coverage of the Ebola (EVD) epidemic in Guinea, Sierra Leone, and Liberia highlighted the public health risks presented by widespread lack of trust in government health workers, who in some cases were suspected of spreading the disease. Given that now the Center for Disease Control website recommends avoidance of hospitals as a key preventive measure, the fact that citizens of the region stay away from their countries’ ill-equipped and poorly sanitized hospitals seems a rational decision, rather than one informed by superstition and baseless rumors. In what follows, I offer my own, ethnographically informed reflections on the challenges faced by rural Sierra Leoneans in accessing the health care system.
When facing illness, many rural Sierra Leoneans display what some might call “fatalism:” ill people and their families often wait in place, consulting healers as much as possible, but not going to hospital, particularly if they judge a person near death. These life and death choices are made by people living on the margins of subsistence in agrarian settings. One of the villages where I have been based, in Wunde Chiefdom, has some 260 inhabitants and is a few miles from a feeder road and without regular transportation. Of the five other villages within a five-mile radius, two are hamlets that can be reached only on foot, and the very ill have to be transported in and out in hammocks strung on a pole.
There are no state health facilities in this village or in smaller neighboring ones. Five miles away, the former headquarter town, Gboyama, has a two-room dispensary for visits during scheduled hours, staffed by a paramedic who occasionally visits outlying communities. These visits are rare, often months apart. This makes a decision to go to the nearest dispensary—let alone hospitals—a physically challenging one for the ill and those organizing their care. Most of the time, rural Sierra Leoneans rely on the expertise of resident herbalists or specialist healers who come to the ill person, instead of requiring him or her to move. Televised images of four-wheel-drive vehicles arriving at the house of an affected victim belie the fact that many rural Sierra Leoneans live in places that are not on motorable roads—one reason health agencies suspect that Sierra Leone may have two to four times the reported EVD cases.
For hospital visits, private transportation needs to be arranged not only for the sick but also for accompanying family members who can buy necessary medications and ensure that the patient is fed and that soiled clothes and bed sheets are laundered. Since the 1980s, public hospitals in Sierra Leone have been so ill-equipped that wound dressings, drugs, antiseptics, catheters, and even stitching materials for surgeries are among the items I have had to purchase for patients I accompanied there. Even purportedly “free” medical care involves expenditures—for supplies, food, transportation—which most Sierra Leoneans factor into their health care choices. Finally, hospitals are crowded places, where individuals can get lost if they do not have advocates to seek care on their behalf, whereas the healer who comes to their bedside gives them undivided attention.
During a May 2012 visit to Wunde Chiefdom, I was presented with three cases that required specialist care: a young man paralyzed by a fall, a boy with a clubfoot, and a man with deep lesions on his legs. I arranged with the boy and his father to meet me at an orthopedic specialist clinic in Makeni and took the other two men to a private clinic in Bo. My friendship with staff there resulted in expedited attention—for a price. We learned that one man’s paralysis was irreversible and that the other was affected by incurable melanoma. As I made arrangements to secure a wheelchair for the disabled man, the doctor whispered that he would have been better off dying in that fall. The comment smacked of fatalism, but it was followed by a concerned analysis of the challenges ahead—a wife and children to support, being in a rural village on hilly terrain, where subsistence depended on work in the fields and it would be difficult to get around even in a wheelchair.
In Makeni we began in outpatient admissions, waiting and then answering questions from a nurse who filled out papers by hand. In another wing of the hospital, we waited for a nurse who screened patients, took vital signs, and issued another piece of paper, then directed us to an office where I could pay in advance for X-rays. We took my growing stack of papers, receipts, and written directions to the radiology department where we waited for the boy’s turn for X-rays, then for another hour for the prints, which we took to the orthopedic specialist’s waiting room. During similar half-days spent in other hospitals, I witnessed nurses and staff congregating for tea breaks, running errands, and transacting private business over cell phones. This is not surprising in light of the need to supplement low wages with other business ventures, but it shapes the perception in patients who are illiterate and unfamiliar with—and intimidated by—the hospital setting that the ethos informing it is more economic than caring.
In the end, the doctor in Makeni determined that surgery was not an option for the young boy because the operating theater was under construction. He noted that the boy seemed to have adjusted to standing and walking with the clubfoot, and he did not want to risk permanently disabling him.
In conclusion, for most rural Sierra Leoneans, getting to hospital involves long, uncomfortable, and expensive journeys, navigating Kafka-esque bureaucracies. Repeated payments are required and long waits are interspersed with inconclusive interactions with medical personnel. After all this, one often returns home as one had left or dies from the journey’s hardships and lack of care. What may appear to be inaction informed by fatalism—even avoidance of proffered medical attention—must be understood as a calculated decision about the costs and benefits of expensive care, based on experience.