Triple Toxicity
From the Series: Embodied Ecologies
From the Series: Embodied Ecologies
A few years into my fieldwork on birth culture in California, I went to meet Harmony at a strip of shops near the beach in Santa Cruz. The coffeeshop was packed and thick with coastal hipness. I ordered a “bowl of soul”—chamomile tea steeped in steamed milk—and staked out a table. We were meeting to discuss the “Mindfulness Childbirth Education” class with which I had assisted early on in my fieldwork. Harmony, a hospital midwife who had trained at the University of California, San Francisco, one of the best medical research hospitals in the United States, was pregnant at the time she took the class. Lexi, the midwife teaching the class, was one of the oldest and best loved midwives in the area, known locally as a pioneer of the birth movement—the revival of natural birth and midwifery, largely among white, middle-class Americans in the 1970s, which had a particularly strong presence in Santa Cruz. Lexi had passed away the month before, and Harmony was preparing to take over teaching her immensely popular class at the hospital where she worked.
Harmony arrived wearing a ponytail, soft grey blouse, and jeans. She carried a bag full of books and apologized for being late; she had had trouble putting her son down for his nap. Over hazelnut cookies and tea, we shared remembered anecdotes and compared notes. Toward the end of the meeting, I recalled that the first time I met Lexi, I asked her if she thought birth has effects that shape a personality, that stay with you throughout your life. “Oh, of course,” Lexi had replied, her lined face breaking into a smile. Harmony agreed, adding: “That’s why I do the work I do!”
Fifteen years ago, she told me, local birth activists had started a now-national group focused on fetal/infant psychological experience. Though parts of the story were familiar to me, Harmony connected them in new ways:
They found out, or they thought, I’m not sure what the research is, but the mom’s stress level determines what kind of egg she releases. If she’s stressed, she produces a being with more emphasis on the midbrain, where the fight or flight instinct comes from, instead of the front brain, where thought and empathy happen. So [a child’s temperament] can start in the mom’s health, even before conception.
I nodded. Harmony continued: “And it makes sense that a lot of cortisol production during pregnancy would make for a highly tuned nervous system in the baby. Cortisol, you know, the stress hormone.” She went on to say that her one-year-old son is jumpier than his peers, probably because she was overworked and stressed out while pregnant. “And that’s not like a war zone or anything,” she said self-deprecatingly. It went without saying between us that the mindfulness classes are related to these claims: mindfulness practice reduces stress, and stress is a toxic affect. The womb is not an impermeable fortress, she implied, but a vulnerable ecology where the psychological capacities of future generations are formed.
Harmony’s take strikes me now, as it did then, as rather unconventional in its bridging of gynecology and psychology, although research does suggest links between oocyte quality and maternal stress (e.g., Prasad et al 2016). Some researchers claim that toxic stress in early childhood detrimentally impacts “the architecture of the brain, the body’s stress response systems, and a host of health outcomes later in life.” Stress, here, is a capacious and naturalized/naturalizing concept that blurs distinctions between material and psychological experience (see Young 1980). Material and psychological fluidities thus link childbearing person and fetus.
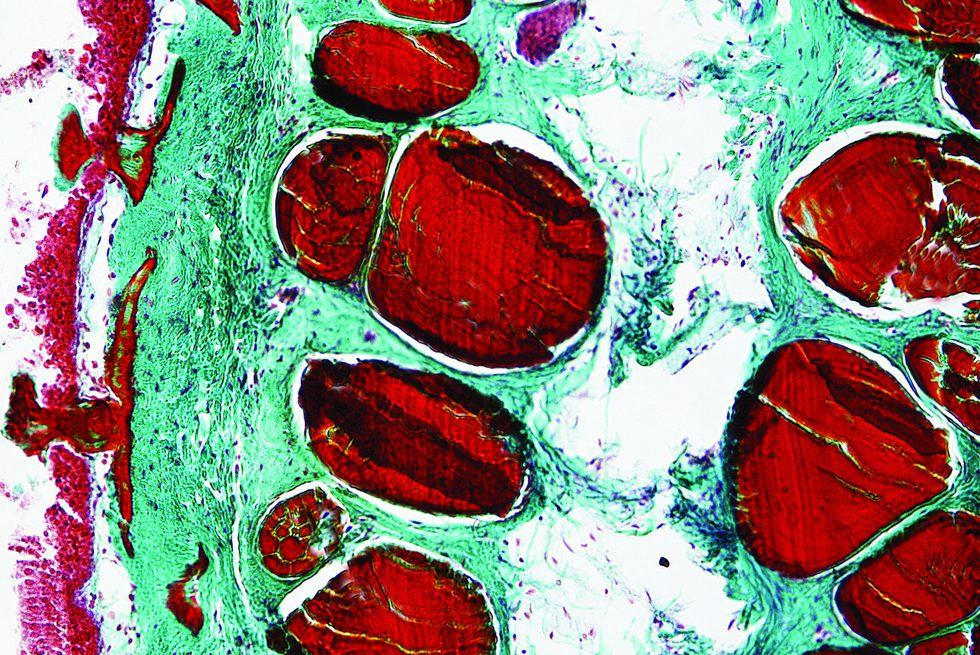
This was not the first time I encountered unconventional ideas about intergenerational well-being during my fieldwork; such ideas circulated in scientific, professional, and popular contexts. For instance, attachment parenting discourse frames infant experience as setting an affective template for life. The maternal microbiome is thought to be passed to the infant during vaginal birth and breastfeeding, processes that if disrupted might lead to poorly “colonized” microbes and, in time, to noncommunicable diseases on epidemic social scales. Postindustrial environments are said to be saturated with chemicals that can be shared through the placenta and breastmilk, disrupting child development and potentially manifesting in epigenetic modifications (Lamoreaux 2016).
I emphasize the similarities of these three things—stress, microbes, and chemicals—because I noticed birth activists talking about them in the same interesting way: one that disrupts the idea of health as a property of an individual human, a condition of either his or her choices or genetic makeup. Instead, I was made aware of a growing lay as well as scientific understanding of health as dependent on environmental factors, dispersed in time and space, interpersonal and partially predetermined generations in advance. In this view, health is an ongoing outcome of the chemical, microbial, and affective ecologies surrounding people and, indeed, composing them.
In childbearing, one body becomes multiple. While this phenomenon privileges thinking about embodied relationality and intertwined health, it also readily slips into a gendered politics of maternal responsibility. Scientific research often frames pregnant women as maternal environments that can impact fetal development, which displaces their own experience and personhood while bolstering discourses of risks for which women are held responsible, even before conception (Waggoner 2017; Valdez 2018). Doing the best thing for one’s baby can lead to a double bind: if you are stressed and pregnant, your baby may suffer lifelong health consequences—but try not to stress about not getting stressed (see Bristow 2014). So it is with some trepidation that I point out how scientific and popular discourse increasingly frames modern environments as disrupting affective, microbial, and chemical ecologies in ways that impact reproduction. I expect to see more medical and political activity around toxic chemicals, toxic (lack of) microbes, and toxic (maternal) affects—a triple toxicity.
Bristow, Jennie. 2014. “The Double Bind of Parenting Culture: Helicopter Parents and Cotton Wool Kids.” In Parenting Culture Studies, edited by Ellie Lee, Jennie Bristow, Charlotte Faircloth, and Jan Macvarish, 200–215. New York: Palgrave Macmillan.
Lamoreaux, Janelle. 2016. “What if the Environment is a Person? Lineages of Epigenetic Science in a Toxic China.” Cultural Anthropology
31, no. 2: 188–214.
Prasad, Shilpa, Meenakshi Tiwari, Ashutosh Pandey, Tulsidas Shrivastav, and Shail Chaube. 2016. “Impact of Stress on Oocyte Quality and Reproductive Outcome.” Journal of Biomedical Sciences 23.
Valdez, Natali. 2018. “The Redistribution of Reproductive Responsibility: On the Epigenetics of ‘Environment’ in Prenatal Interventions.” Medical Anthropology Quarterly 32, no. 3: 425–42.
Waggoner, Miranda. 2017. The Zero Trimester: Pre-Pregnancy Care and the Politics of Reproductive Risk. Oakland: University of California Press.
Young, Allan. 1980. “The Discourse on Stress and the Reproduction of Conventional Knowledge.” Social Science and Medicine, Part B 14, no. 3: 133–46.