Covid-19 and Tibetan Medicine: An Awakening Tradition in a New Era of Global Health Crisis
From the Series: Responding to an Unfolding Pandemic: Asian Medicines and Covid-19
From the Series: Responding to an Unfolding Pandemic: Asian Medicines and Covid-19
Days after news hit the Tibetan plateau of the novel coronavirus outbreak in Wuhan, provincial health bureaus and central Tibetan medical institutions across the region launched official protocols1 for prevention, treatment, and rehabilitation in preparation for cases of infected patients. Senior physicians published statements instructing junior colleagues,2 and permeated social media with their public health education presentations, interviews, and lectures. In professional and public talks, including by Harvard alumnus Yang Ga and UCLA Public Health graduate Kunchok Gyaltsen, it became apparent that the emergence of SARS-CoV-2 presented not only a major national health crisis, but simultaneously opened up possibilities for a new emerging public face of Sowa Rigpa (Tibetan medicine, the “Science of Healing”)—a stark contrast to decades earlier.
China officially classifies Tibetan medicine as “Traditional Chinese Medicine,” a contemporary umbrella term encompassing all its ethnic medical traditions. Such policy risks absorbing Sowa Rigpa into this larger category, making it invisible to the greater public. This article argues that Tibetan physicians are collectively transcending this limitation by building status for their tradition in this global era. Covid-19’s pandemic provides a critical window to track Sowa Rigpa’s scope and impact in China at this time. China’s almost exclusive social media application, WeChat, provides detailed time points of Tibetan medical responses to the pandemic. WeChat is now a mainstream source of transregional news, events, and broadcasts, as well as data and publication sharing.3 This piece uses such methods, in addition to reviewing publications, online sources, and personal communications.
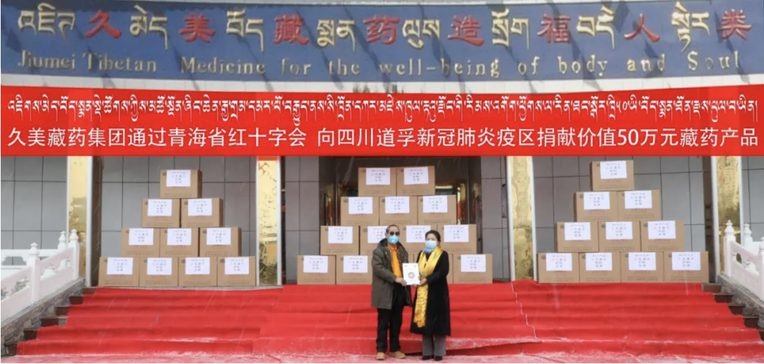
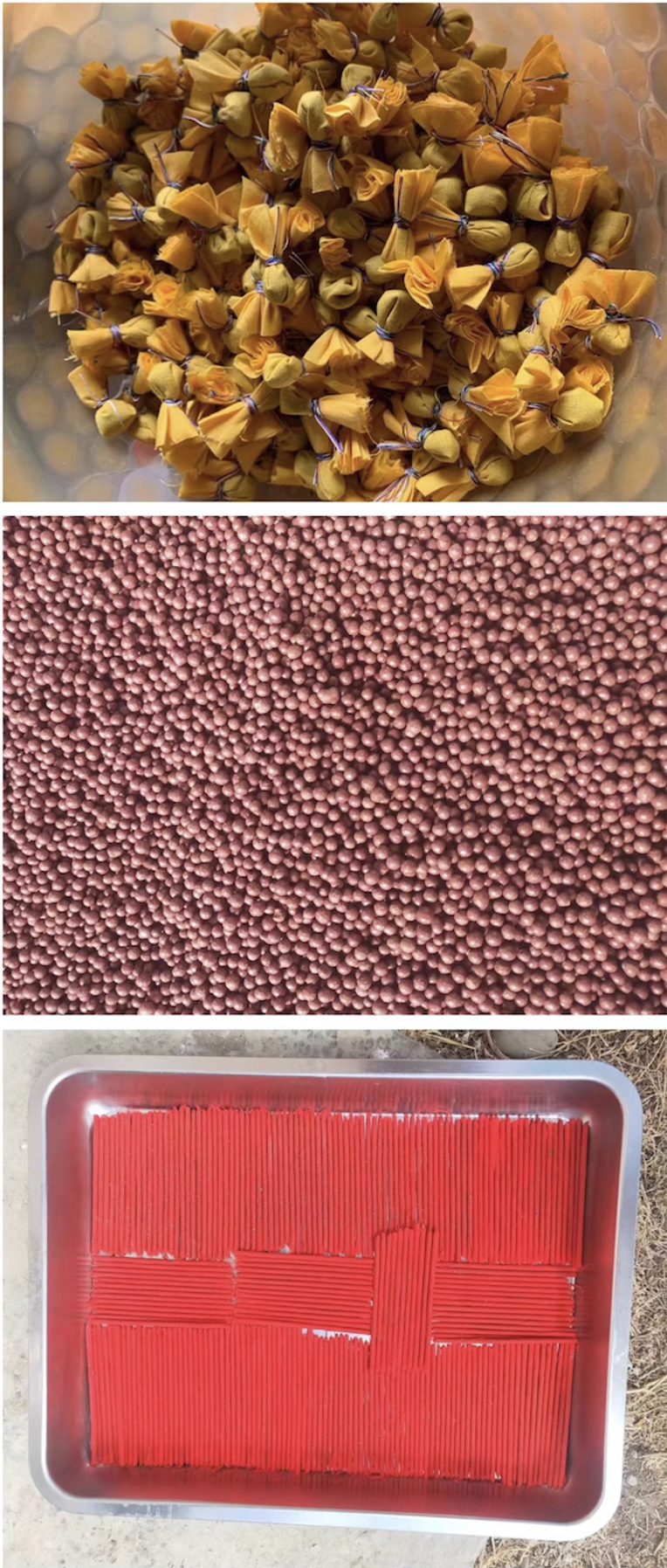
As their expertise flooded the virtual landscape in early January (see Tomar and Sheldon, this series, for virtual responses in Ayurveda), Tibetan physicians also sent workers and large supplies of respiratory and infectious disease medicines to affected areas in mainland China, including Wuhan.4 Externally worn sachets of the Nine-Compound Black Pill, traditionally described for protective qualities, were also mobilized. Shipments launched from Lhasa Mentsikhang, Qinghai Provincial Tibetan Medical Hospital and various prefecture, county, and private producers (Dhondrup et al. 2020). Although government regulations limited acceptable relief donations to formulas meeting national good manufacturing practice standards, contributions still amassed worth tens of millions RMB. Likewise, restrictions on traditional medicine permitted in biomedical institutional treatments also constrained formulas to mild cases.5 Qizheng, China’s biggest Tibetan pharmaceutical producer also sent its licensed formulas6 to Wuhan, Beijing, and its home Gansu hospitals.7
Though Lhasa’s first reported case
was not until January 25, 2020, by February 25, Tibetan regions had significant transmission—with the greatest concentration in Kardzé Prefecture and, in particular, its far eastern Tawo County.8 Donations from plateau sources shifted local relief to target Tibetan communities.9 Prominent private Xining physician Jigmé Puntsok contributed half a million RMB (US$70,565) worth of one of his nationally certified formulas, Red Tazi.10
Even in areas with no reported cases, physicians donated protection substances, such as the Nine-Compound Black Pill and Epidemic Protector amulets (see Gerke, this series), to their local communities, simultaneously providing virus education outreach and encouraging stringent health protection measures.
Despite some criticism within the field, such as Southwest Minzu University Professor Emeritus Thupten Phuntsok accusing Tibetan physicians of exploiting crisis to make profit on amulets and preventative substances, and claiming mantras are meaningless during epidemics, provincial to township level physicians and institutions liberally donated time and resources. Several hospitals even provided free care to confirmed cases. Whether Thubten Phuntsok’s comments incited greater charity is difficult to determine—but regardless, generosity unfolded substantially.
The Tibetan medicine industry has grown significantly over the last few decades, reaching one billion U.S. dollars in production by 2018 (Kloos et al. 2020). The richness of tradition, proficiency, and rigor put forth in this contemporary context could not be demonstrated decades earlier, when Tibetan medicine was under heavy scrutiny from the central Chinese government to appear biomedical and non-religious (Janes 1995). After the initial Democratic Reforms (1959–1962) and the Cultural Revolution (1966–1976), the period following Mao’s death led to cautious expansion and legitimization efforts among Tibetan physicians. Sowa Rigpa institutions stripped any Buddhist or Tibetan cultural references from their medical curriculum and instead framed medical content in biomedical terms (Adams and Li 2008). In the post-reform era, state funding transformed Tibetan medical institutions into partial replicas of biomedical counterparts. For compliance, Tibetan physicians consciously reframed disease causation explanations in explicitly biomedical terms.
Recent decades, however, have seen a new wave of central government support for ethnic minority medical traditions, and explicit legislation supporting their role in combating common diseases, chronic conditions, and epidemics.11 Xi Jinping’s advocacy for traditional culture and integration of ancient Chinese philosophy has created a rhetorical distance to a time when Mao attacked Confucian ideas, erasing them with revolutionary fervor. Today, nostalgic for tradition and eager for rehabilitation, public discourse has situated Tibetan medicine in a politically favorable climate to regenerate tradition and expand medical practice and scope, though still forcing physicians to walk a fine line with religious practice. By 2019, Qinghai Province procured funds, built and staffed Sowa Rigpa facilities at every administrative level,12 such that “access to healthcare provided by Tibetan medical institutions now outnumbers that of biomedical clinics across the province.”13 Before 1950, Sowa Rigpa was virtually the only form of healthcare on the Tibetan plateau (Hofer 2018). Redeveloping Sowa Rigpa so that it features centrally as the primary healthcare system in Tibet, even expanding it beyond its historical reach, is eagerly welcomed by Tibetan physicians and the communities they serve. This represents a departure from decades of historical relegation of Tibetan medicine to inferior status and widespread Tibetan distrust of Chinese institutions and physicians. It also provides space for cultural expression, addressing community health needs, and cultural sensitivity in treatment.14
A “crisis of confidence” decades prior (Craig 2007), when Tibetan physicians questioned their competence alongside biomedical peers, has segued into engagement where today, in the PRC, most Tibetan medical and education bodies work in tandem or full integration with biomedical colleagues through partnership and cross-training. Many Tibetan physicians gain insight into the weaknesses as well as strengths of biomedicine, and are able to emphasize Sowa Rigpa’s unique contributions.15 Neuroscience research has generated insights on health benefits related to practices of Tibetan Buddhist expert meditators (Lutz et al. 2008; Kaliman et al. 2014) and derived mindfulness interventions (Rosencranz et al. 2016). Alongside China’s Buddhist revival, with mainland Chinese also seeking Tibetan Buddhist teachers (Hardie 2018), these influences give Tibetan medical professionals confidence to more openly discuss Buddhist practices in relation to medicine. Physicians recommend visualizations, compassion meditations, mantra recitation, amulets, and tantric ritual practices even to mainland Chinese patients. Such methods would not have been openly discussed or advised decades ago.
As news of containment in Wuhan spread, Qinghai Provincial Tibetan Medical Hospital reported on Xining’s recovered cases, accepted for post-recovery care at their hospital under their developed protocols. Tawo County reports also emerged on cases treated successfully with integrated biomedical-Tibetan medical care, making their physicians cultural heroes.16

News circulated that only one of a thousand Tibetan students in Wuhan had confirmed viral contraction. Many Tibetans attributed this news to precious pills, mani rilbu,
and other Tibetan medical preventative measures.17
Amid these reports, Zhong Nanshan, China’s chief coronavirus expert announced the national Covid-19 research committee’s interest in Tibetan medical approaches to mild cases due to preliminary efficacy evidence
and potential insights from a history in high altitude hypoxic environments. Zhong Nanshan also announced a research collaboration
with Qizheng Tibetan pharmaceuticals, launching a forty-subject clinical trial in Wuhan using three of Qizheng’s nationally approved formulas. While they collect data, a preliminary auxiliary report recommends adjunct use of Tibetan therapies in biomedical hospitals to reduce mortalities (Dhondrup et al. 2020, 8). Local plateau research institutions also recently received national funds to expand related studies.18
Tibetan physicians have skillfully navigated challenging historical conditions (including points of potential erasure) and contemporary circumstances regulating participation. By mobilizing in this novel crisis context, they demonstrate an awakening tradition within an increasingly global integrated health landscape.
The research and writing of this article were supported by the Center for Healthy Minds [project number AAG8698] at University of Wisconsin-Madison.
1. With a team of experts guiding each province, the Tibetan Medicine Administration of the Tibetan Autonomous Region (TAR) launched their protocol on January 26, 2020; Qinghai Provincial Health Bureau on February 1; Kardzé Autonomous Prefecture of Sichuan Province on February 10; and Gansu Provincial Health Department on February 15. Protocol measures recommended include dietary and behavioral practices, as well as medicines for prevention. Treatment guidelines were delineated for elderly, children, and adults distinctly, and with 25, 14, 3, and 3 formulas, respectively for each province. Second editions of protocols were published later for the TAR on February 23 adding eleven more medicines; for Qinghai on February 24 adding ten more medicines, and subsequently by Kardzé Prefecture and Gansu adding formulas to their respective protocols as well. Some of the formulas common to the protocols include: Norbu 7 Tang, Trültang, Logyönma, Tsowo 25, Lotsé Künsel, Red Tazi, and Mangjor precious pills (Dhondrup et al. 2020, 4–6).
2. In addition to decoction formulas, precious pills and externally adorned sachets were recommended for prevention. In the primary care instructions on Covid-19, Tibetan physicians outlined the first line of Sowa Rigpa formulas that should be prioritized for treating initial symptoms at the point of disease inception called “unripened fever” (Tib. ma smin tsha ba) and progressing into more aggressive formulas if the condition develops to full manifestation (rgyas tshad, stongs tshad) to support the immune system, lower inflammation, improve lung function, support digestive capacity, and improve overall physical strength. The classical terms used in the protocol read, “First, demolish the mountain of virulence, then extinguish the flames of fever, and finally treat the winds and rehabilitate the body” (dang po gnyan gyi ri bo bsnyil/ bar du tshad pa’i me dbal bsad/ tha mar rlung bcos lus po gso/ [TAR 2020, 5]). In circulated guiding documents, senior physicians also include instructions to the public on the most helpful mantras to recite, amulets to wear, and contemplative practices in which to engage.
3. Kunchok Gyaltsen, Encountering COVID-19: Perspectives from Tibetan Medicine Webinar Series, April 19, 2020.
4. Formulas sent as relief include Trültang, Logyönma, Red Tazi, and Mangjor precious pills (Dhondrup et al. 2020, 4–6).
5. Personal communication, Rinchen Dhondrup, April 9, 2020; Kunchok Gyaltsen, Encountering COVID-19: Perspectives from Tibetan Medicine Webinar Series, April 19, 2020.
6. With national authorization to distribute many of its formulas to biomedical hospitals, it sent Logyönma, Rinchen Mangjor, and Trültang decoction formulas (Dhondrup et al. 2020, 5)
7. Gansu Province hospitals are particularly known for extensive use of integrative medical protocols. Personal communication, Mingji Cuomu, April 9, 2020.
8. Of the 78 confirmed cases in Kardzé Tibetan Autonomous Prefecture on March 6, 2020, one report mentions 61 cases were in Tawo County (Dhondrup et al. 2020, 6), one report mentions 73 (Phuntsok Dorjé, Encountering COVID-19: Perspectives from Tibetan Medicine Webinar Series, April 19, 2020)
9. Dergé and Chaktreng—counties adjacent to Tawo, distant sources such as Nyingri (TAR), and private philanthropists contributed (Dhondrup et al. 2020, 7).
10. Jigmé Puntsok produces 322 formulas in total, but only fourteen have national authorization for use in mainland hospitals. Red Tazi is described for its benefits in fighting respiratory and brain infection, as well as systemic inflammation in the form of fevers (Ridak 2003).
11. As quoted from Article 14 of “People’s Republic of China Statute for Use of Traditional Chinese Medicine Pharmaceutical Compounds” (Dhondrup et al. 2020, 8).
12. Personal communication, Drotsang Dhondrup, May 23, 2020.
13. Qinghai Provincial Heath Bureau Ethnic Traditional Medicine Division Director
14. Personal communication, Takdruk Tserang, June 15, 2019.
15. An example here are the Lhasa-based Tibetan physicians who composed the application to UNESCO for Intangible Cultural Heritage recognition of Lum Medicinal Bath.
16. The report by Dhondrup and colleagues details the efforts of Kardzé Prefectural People’s Hospital and Tawo County People’s Hospital in collecting case studies and comprehensive data of fully treated confirmed Covid-19 cases by integrative medicine means, but did not release the results yet (Dhondrup et al. 2020, 6).
17. Note that it is unknown if there were asymptomatic cases, since those who did not exhibit symptoms were not tested.
18. Lhasa Mentsikhang, with its partner the Tibetan Medical Research
Institute, were recently awarded 500,000 RMB (approximately US$70,500). Qinghai Provincial Tibetan Medical Hospital also received 650,000
RMB (approximately US$91,700) to initiate research on Nine-Compound
Black Pills both for investigating therapeutic effects and
pharmacological qualities. Qinghai’s largest Tibetan pharmaceutical
company Arura Group was also awarded similar research funds to
investigate infectious disease control measures in Tibetan medicine
(Dhondrup et al. 2020, 7).
Adams, Vincanne, and Fei-Fei Li. 2008. “Integration or Erasure? Modernizing Medicine at Lhasa’s Mentsikhang.” Tibetan Medicine in the Contemporary World: Global Politics of Medical Knowledge and Practice, edited by Laurent Pordié, 105–30. London: Routledge.
Craig, Sienna R. 2007. “A Crisis of Confidence: A Comparison Between Tibetan Medical Education in Nepal and Tibet.” In Soundings in Tibetan Medicine, edited by Mona Schrempf, 127–54. Leiden: Brill.
Dhondrup, Rinchen, Dekyi Tsomo, Nyargyal Tsen, Buchung Tsering, and Rinchen Gyal. 2020. “Bod kyi gso ba rig pas tog dyibs nad dug gsar pa’i glo tshad rims nad ’gog bcos thad gal che’i nus pa thon tshul” [Guidance Document of Emergent Findings for Tibetan Medicine’s Efficacy to Prevent and Treat Respiratory Infections of SARS-CoV-2]. Unpublished report manuscript.
Hardie, Catherine. 2018. “Tibetan Buddhist Spiritual Capital in Contemporary China.” PhD diss., School of Anthropology, University of Oxford.
Hofer, Theresia. 2018. Medicine and Memory in Tibet: Amchi Physicians in an Age of Reform. Seattle: University of Washington Press.
Janes, Craig R. 1995. “The Transformations of Tibetan Medicine.” Medical Anthropology Quarterly 9, no. 1: 6–39.
Kaliman, Perla, María Jesús Alvarez-López, Marta Cosín-Tomás, Melissa A. Rosenkranz, Antoine Lutz, and Richard J. Davidson. 2014. “Rapid Changes in Histone Deacetylases and Inflammatory Gene Expression in Expert Meditators.” Psychoneuroendocrinology 40: 96–107.
Kloos, Stephan, Harilal Madhavan, Tawni Tidwell, Calum Blaikie, and Mingji Cuomu. 2020. “The Transnational Sowa Rigpa Industry in Asia: New Perspectives on an Emerging Economy.” Social Science and Medicine 245: 112617.
Lutz, Antoine, Julie Brefczynski-Lewis, Tom Johnstone, and Richard J. Davidson. 2008. “Regulation of the Neural Circuitry of Emotion by Compassion Meditation: Effects of Meditative Expertise.” PLoS ONE 3, no. 3: e1897.
Ridak, Dawa. 2003. Bod kyi gso ba rig pa las sman rdzas sbyor bzo’i lag len gsang sgo ’byed pa’i lde mig [Key to Unlocking the Secret Door of Medicine Manufacturing Practices of Tibet’s Sowa Rigpa]. Delhi: Rig Drag Publications.
Rosenkranz, Melissa A., Antoine Lutz, David M. Perlman, David R. W. Bachhuber, Brianna S. Schuyler, Donal G. MacCoon, and Richard J. Davidson. 2016. “Reduced Stress and Inflammatory Responsiveness in Experienced Meditators Compared to a Matched Healthy Control Group.” Psychoneuroendocrinology 68: 117–25.
TAR (Tibet Autonomous Region Tibetan Medicine Administration). 2020. Bod rang skyong ljongs gsar ton tog dbyibs nad dug rang bzhin gyi glo tshad bod lugs gso rig gi ‘gog bcos jus gzhi [Tibet Autonomous Region Strategic Plan for Tibetan Medicine Prevention and Treatment of Pulmonary Inflammation Caused by Novel Coronavirus]. Bod rang skyong ljongs bod lugs gso rig do dam cus kyi yig cha, March.